Picture this: you have an appointment with a dermatologist to discuss acne treatments. For the paperwork, you have to use a name that isn’t yours, and makes you uncomfortable when people use it and say that you’re a woman on paper, even though you aren’t. Nowhere does it ask if you go by another name, even a nickname, and when you arrive, the wrong name is used repeatedly, and people keep calling you “she” and “her.” When you’re taken back to see the doctor, they ask what medications you’re on. You don’t want to leave anything out, so you say it.
“Testosterone.”
The doctor raises an eyebrow, and instead of asking you what to call you or how you’d like to be referred to, he makes assumptions and begins a spiel about how you’ll never be able to fully treat your acne since as long as you’re on hormones, you’re in an eternal “puberty,” and the only option is Accutane, which requires a monthly pregnancy test. While this diagnosis has some merit, such a snap assessment isn’t true.
Since I started my transition and journey as a transmasculine (a term used for those assigned female at birth who lean towards being more masculine-identified, but not necessarily a man), nonbinary individual, I have had countless interactions with doctors, other health professionals, and staff along these lines.
It’s experiences like this that make trans folks around the world feel alienated and alone every day. For trans women, trans men, and people who identify elsewhere off the spectrum, the experience is often similar. A glaring lack of trained professionals is evident, and while many have good intentions, it can be tempting to avoid medical care whenever possible.
Shedding Light on Transgender Healthcare Services in the United States
The United States faces a significant deficiency in comprehensive and educated health professionals, particularly doctors, when it comes to transgender healthcare. Despite strides (and steps back) in societal understanding and acceptance of diverse gender identities, the medical field has lagged in providing adequate training and education on transgender-specific health issues.
Many healthcare providers lack the knowledge and cultural competence necessary to deliver affirming and effective care to transgender individuals. The consequences of this gap are profound, as it contributes to the perpetuation of health disparities and barriers to accessing essential services.
Healthcare settings and practitioners generally emphasize “men’s health” or “women’s health,” overlooking gender-diverse individuals. Registration forms typically lack options for indicating a gender identity distinct from the assigned sex at birth, and health screenings and insurance policies are based on a binary male-female model, neglecting the needs of gender-diverse patients.
Medical education is affected by societal biases, sometimes leading to stereotypes and prejudices by medical students. Only 26% of doctors overseeing family medicine clerkships feel comfortable teaching transgender healthcare to students.
Recognizing this deficiency, the Association of American Medical Colleges advocates for a comprehensive approach to LGBTQ+ health education at all levels of medical training. It suggests a “layered” strategy, integrating gender-affirming healthcare education throughout the curriculum. However, many medical schools still fall short of incorporating such care seamlessly, often resorting to add-on approaches like standalone lectures or small-group activities. On average, medical schools provide just five hours of instruction on gender-affirming healthcare practices, highlighting the lack of comprehensive training in this crucial area.
Lack of Educated Doctors Equals Avoidance of Treatment
Another instance of incompetent care I experienced was in 2021 when I received top surgery (subcutaneous mastectomy, male/masculinizing chest contouring) through Kaiser Permanente in Denver.
My surgeon was well-intentioned and really took the time to listen, inspired by her trans best friend to provide comprehensive and continually improving care. However, despite her best efforts, many other staff fell far short of her level of understanding.
After completing the World Professional Association for Transgender Health or WPATH screening (a grueling process trans folks have to complete by answering questions with a licensed therapist to prove that their care is necessary) and having many appointments up until the surgery, I arrived the day of the surgery and was called every pronoun under the sun, mostly incorrect — I use they/them — when my surgery team should have been prepped on what to call me.
My partner was also misgendered through my surgery and their own about six months later by the same team for the same procedure. Of course, people make mistakes, and I don’t expect perfection, but I expect some level of effort when receiving care.
Due to limited training on gender-affirming care during medical education, gender-diverse individuals often find themselves educating their primary care providers. I have found myself in the position of teacher instead of simply being a patient over the years. This deficiency in understanding and provision of competent care has significant consequences, with one in three gender-diverse adults avoiding preventive care or not being offered such services. Alarmingly, 19% of transgender individuals report being outright refused care.
These disparities may contribute to the higher rates of tobacco use, obesity, alcohol consumption, depression, and cancer risk factors among gender-diverse populations.
With so much stress surrounding being transgender already, I know many people who will outright avoid going to the doctor and instead get hormones and even services without safe consultation, relying on more shady methods such as buying from a friend who has a prescription or even relying on illegal and risky sources.
I know a trans woman, for instance, who went in to see her doctor and disclosed at the beginning of the appointment that she was trans and hadn’t yet had bottom surgery. They got through most of the exam, talking about how she had been buying unused hormones from other trans women and how she wanted to start her transition properly with a doctor. After this whole conversation, the doctor told her to prep for a pap smear, leading to an awkward experience for both of them when the doctor should have known that wasn’t something physically possible to provide yet.
Transgender Health Services are Life Saving
A 2020 study in The American Journal of Psychiatry revealed that transgender individuals who underwent gender-affirmation surgery experienced an 8% reduction in the likelihood of seeking mental health treatment each year post-surgery. This surgery also brought about various positive effects, such as improved self-image, enhanced sexuality, sexual satisfaction, and increased social affirmation, contributing to a better quality of life.
I know many people who have struggled emotionally with depression and suicidal ideation while awaiting surgeries and care around their identities. While gender-affirming services aren’t a cure-all, they greatly increase quality of life once completed.
Despite these evident health benefits, a substantial knowledge gap exists among physicians when it comes to caring for transgender patients. Many doctors lack training in gender-affirmation procedures, leading to inadequate care, especially when complications arise from these surgeries. This gap is particularly problematic since trans patients often seek surgery in states where such procedures are legal, yet aftercare is managed by primary physicians unfamiliar with transgender care. This overall lack of awareness and training can significantly impact the outcomes for trans patients.
When I started hormone replacement therapy in 2019, I started with Plume Health (when it was still called Mariposa), a trans-led healthcare company that offers discreet hormone prescriptions and monitoring for $100 a month. Initially, the company didn’t accept insurance, but I didn’t want to use insurance anyway for safety purposes within my family. Now, Plume offers its services for $40/month with qualifying insurance, but even with that, care like this is often out of reach financially. You shouldn’t have to go somewhere special to get the care you deserve that will likely change the course of your life for the better.
The barriers are manyfold, whether it be uneducated doctors, the WPATH process, getting good therapists, financial roadblocks, etc. These services are guarded, and they make sure you really need it before it’s provided. Only about 3% of adults who transition end up de-transitioning.
How Can We Do Better?
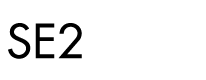
So, what can be done to help address this issue? Behavior change marketers can be crucial in addressing the lack of trauma-informed, culturally relevant, and trans-specific healthcare by implementing targeted strategies that promote awareness, education, and inclusivity. (Similar progress, of course, must be made in closing broader health inequities).
For trans-specific health care, I recommend:
- Creating inclusive messaging:
- Develop messaging that is inclusive, respectful, trauma-informed, culturally diverse, and affirming of gender identities and sexual orientations for doctors and healthcare professionals.
- Collaborating with advocacy groups and healthcare professionals
- Work closely with LGBTQIA+ advocacy groups, healthcare professionals, and organizations to gain insights and collaborate on creating effective campaigns.
- Creating educational campaigns
- Develop educational campaigns that raise awareness about trauma-informed care, cultural competence, and trans-specific healthcare needs for doctors and healthcare professionals, as well as transgender individuals and allies.
- Helping facilitate and encourage training for healthcare providers
- Invite healthcare providers who are knowledgeable and sensitive to the community’s needs to offer training sessions to increase their peers’ understanding of trans-specific healthcare needs.
- Using positive role models and testimonials
- Highlight positive stories and testimonials from individuals within the trans communities who have had positive healthcare experiences to inspire and encourage individuals to keep medical care.
- Showcase diverse role models within the healthcare field to inspire confidence and trust in providing the correct care to the community.
- Addressing systemic barriers
- Advocate for policy changes and institutional practices to eliminate systemic barriers to trauma-informed, culturally relevant healthcare and ensure inclusive healthcare policies.
- Providing accessible resources
- Develop easily accessible resources, such as brochures, online materials, and helplines, that offer information on trauma-informed, culturally relevant, LGBTQIA+, and trans-specific healthcare services for doctors, healthcare workings, and patients.
By employing these strategies, we can create a more inclusive and supportive healthcare environment and happier, healthier patients.

About the Author:
RJ Johnson (they/them) creates fun, engaging, and strategic content. They enjoy creative strategy, experimenting with content ideas, and storytelling. With over five years of experience in marketing, communications, and content management, they have touched just about every aspect of the field. A lifelong learner, RJ has an M.B.A. from the University of Colorado, Denver, and a B.F.A. in Creative Writing from Stephens College. RJ comes to SE2 from the health insurance sector and is passionate about aiding in the fight for equal opportunities and advocacy. They approach everything from a lens of intersectionality and community.