Consumers love it.
When it comes to consumers, the data-driven wave is ready to crest.
Consumers are plugging in to personal health trackers at record rates. According to a report by Juniper Research, the market is projected to grow 366 percent by 2017.
Payers are embracing it.
My employer benefited from the data-driven employee health program, too. A healthier workforce lowered costs for insurance and decreased associates’ need for expensive procedures.
But is it a winning recipe for providers?
Providers can win with big data too, but it takes a thoughtful approach.
Where we go from here?
The Obama workgroup’s report ends with an acknowledgement that the insights must be considered in other administration policy priorities.
Tip Sheet
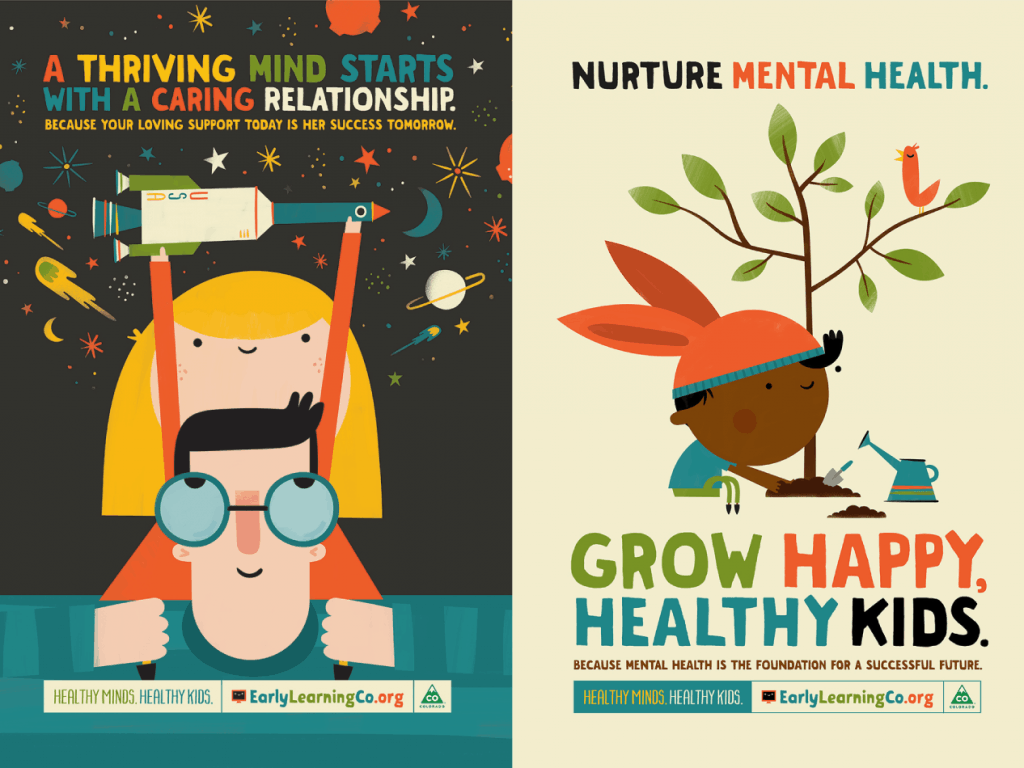
Using Technology to Deliver Targeted Health Messages
Improve health outcomes and your bottom line